Artificial intelligence transforms the stethoscope into a precise diagnostic tool for heart disease – and could fundamentally change the early detection of heart failure, atrial fibrillation and heart valve defects.
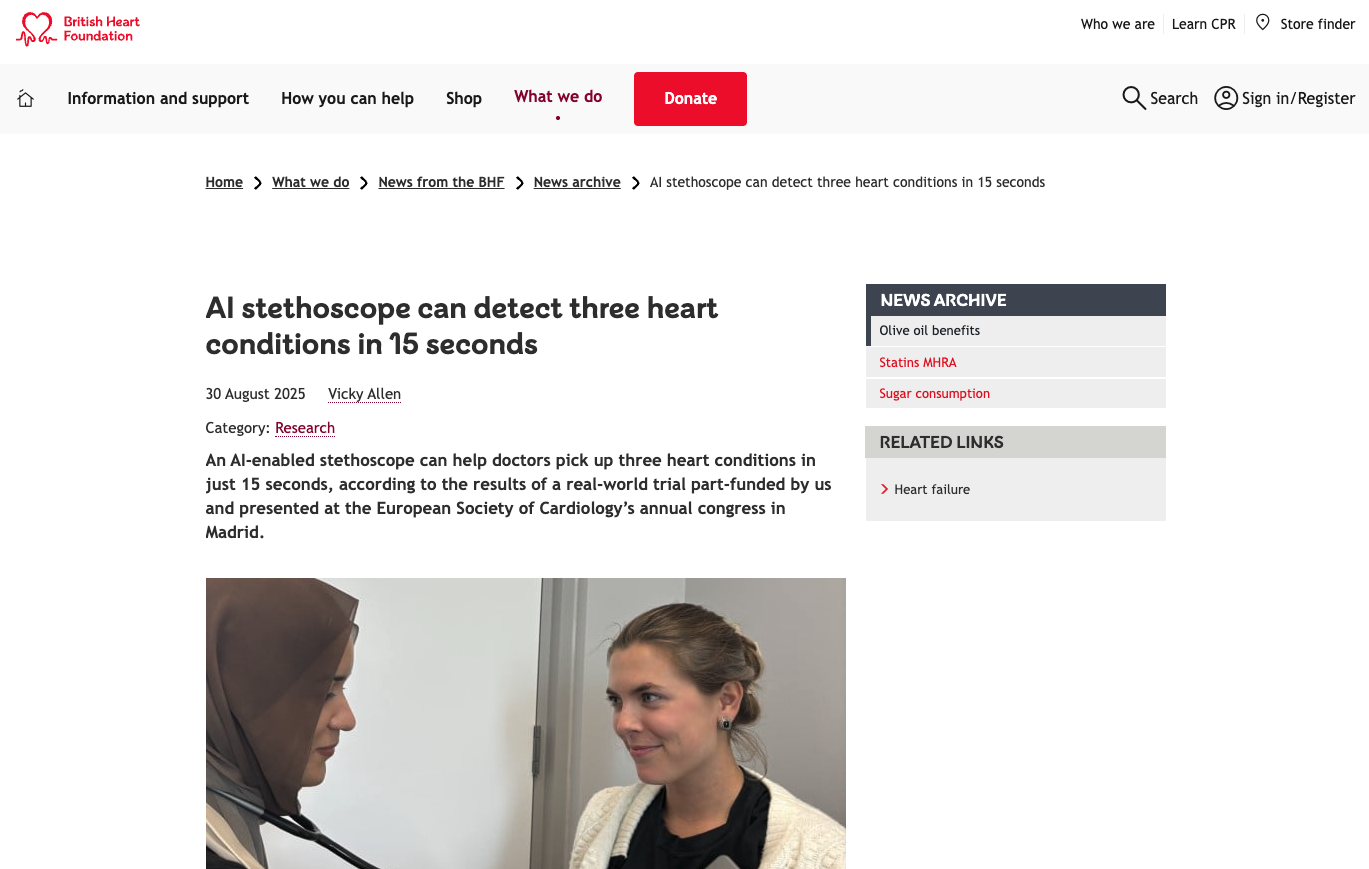
A pioneering study by Imperial College London shows impressive results: AI-powered stethoscopes can identify three critical heart conditions in just 15 seconds. The study involved over 1.5 million patients in more than 200 GP practices and documented dramatic improvements in diagnosis. Patients screened with AI stethoscopes were 2.33 times more likely to be diagnosed with heart failure, 3.45 times more likely to be diagnosed with atrial fibrillation and 1.92 times more likely to be diagnosed with valvular heart disease.
The device, which is about the size of a playing card, combines highly sensitive digital microphones with ECG sensors and uses cloud-based algorithms that have been trained with health data from tens of thousands of patients. This technology detects subtle heart rhythm variations and blood flow dynamics that are imperceptible to the human ear. The results are transferred to a smartphone or tablet within seconds and enable immediate clinical decisions.
Challenges in practical implementation
Despite the convincing study results, clinical implementation presents a complex picture. It is noteworthy that 70 percent of the participating GP practices stopped using the AI stethoscopes regularly after 12 months. In addition, two thirds of patients classified by the system as suspected of having a weak heart turned out to be healthy on further examinations – a high false-positive rate that entails additional diagnostic procedures and costs.
Workflow integration is a particular hurdle. Although the analysis only takes 15 seconds, device set-up, patient positioning and result interpretation require additional time in already tight consultations. GPs have to weigh up the added value of this investment against the practical limitations, especially when suspicious findings result in further costly investigations and specialist referrals.
Economic considerations and future prospects
Cost-benefit analyses conducted by the Mayo Clinic yielded promising results: The incremental cost-effectiveness ratio is $27,858 per quality-adjusted life year, and as low as $1,651 in outpatient settings. These values are well below the thresholds for cost-effective health interventions and take into account long-term savings from earlier diagnosis and treatment.
International validation of the technology demonstrates its global applicability. A Mayo Clinic study in Nigeria to detect pregnancy-related heart failure identified twice as many cases as conventional screening methods. Doctors were twelve times more likely to detect weak heart function with ejection fractions below 45 percent using AI technology. These successes in resource-limited settings demonstrate the potential to reduce health inequalities worldwide.
Executive Summary
- AI-powered stethoscopes improve diagnosis of heart failure by a factor of 2.33, atrial fibrillation by a factor of 3.45 and valvular heart disease by a factor of 1.92
- The technology combines digital microphones with ECG sensors and cloud-based algorithms for 15-second analysis
- Implementation barriers led to 70% of GP practices discontinuing use after 12 months
- High false-positive rate of two-thirds for suspected heart failure cases requires costly follow-up tests
- Cost-effectiveness analysis shows favorable ratio of $1,651 per quality-adjusted life year in outpatient settings
- International studies in Nigeria demonstrate successful use in pregnancy-related heart failure with double detection rates
Source: British Heart Foundation